Histamine degradation disorder / Histamine intolerance / Mast Cell Activation Syndrome (MCAS) / Mastocytosis
Increasingly, individuals are coming to us with histamine-associated conditions. It is therefore of particular concern to me to inform about this topic. The reason for this increase is ultimately not fully clear, but the increase and diversity of symptoms is pronounced and without a doubt.
We are seeing an increased frequency of mast cell activation syndrome (MCAS) following coronavirus infections and also following coronavirus vaccinations as part of a POST VAC syndrome. Although MCAS is a medical condition recognized in the field of medicine, it is often not well understood in traditional outpatient and inpatient DRG medicine (a DRG code is assigned to each diagnosis with an optimal length of stay for optimal reimbursement). There is a widespread lack of knowledge and patients are often stigmatized as having a mental illness.
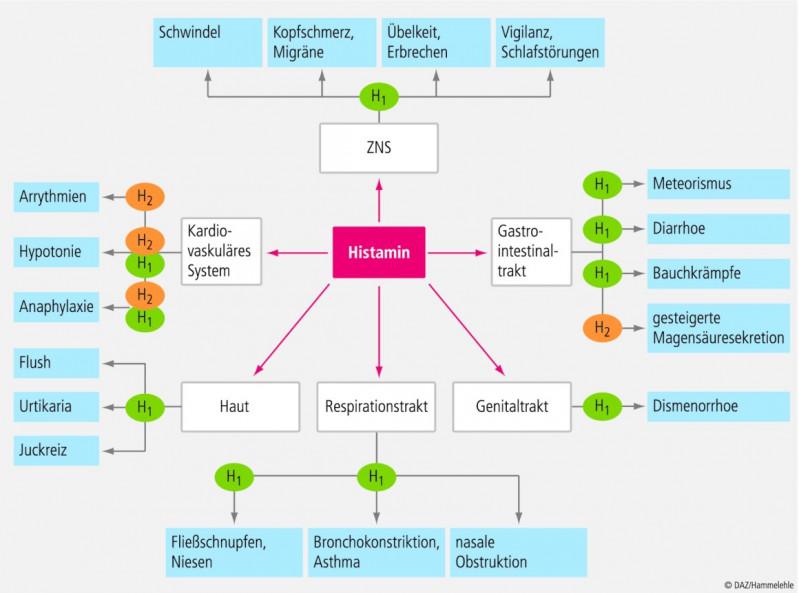
We now want to examine different presentation patterns of symptoms associated with histamine, as shown in the following graphic. The diagram below shows histamine-associated complaints, broadly simplified, through H-1 and H-2 histamine receptors.
Differentially, we clarify histamine degradation disorders, an increased formation of histamine in the intestine as well as a mast cell activation syndrome or a mastocytosis (the latter is very rarely present).
Histamine intolerance or degradation disorder: Symptoms
Histamine is an ubiquitous neurotransmitter, and as a result, disorders of the histamine metabolism can affect a wide range of organs (skin, cardiovascular system, heart, central nervous system, gastrointestinal tract, uterus, lungs, bronchi, etc.).
Psychiatric symptoms are also caused, among other things, by disturbances in histamine metabolism (keyword: histadelia). Histadelia is manifested, for example, by the following symptoms: Maladaptive sensations, delusions, compulsive acts, disturbances in the flow of thoughts, absent-mindedness, abnormal fears, constant suicidal depression, rapid onset of tears, and confusion. It is estimated that 20% of patients with schizophrenia suffer from histadelia.
Furthermore, complaints often occur in the gastrointestinal area (heartburn, stomach pain, ulcers, food intolerances or allergies, etc.) , Skin diseases (e.g. hives, eczema, etc.), respiratory problems (e.g. asthma), neurological disorders (migraine, ADD, ADHD, schizophrenia, chronic fatigue, headaches), gynecological complaints (especially problems occur around the 15th day of the cycle and shortly before menstruation, premenstrual syndrome, cycle-dependent migraine) and dizziness.
It often takes many years to reach a correct diagnosis, and most affected individuals have already suffered for quite a while. They are often falsely labeled as psychosomatically ill. Histamine acts through three different receptors, H1, H2, and H3 receptors. These receptors are present almost everywhere, explaining the diverse symptoms of histamine excess in the body.
Histamine intolerance or degradation disorder: Causes
A histamine intolerance or impaired histamine degradation can be primarily or secondarily caused (primarily = genetically / HNMT or DAO polymorphisms or secondarily due to a coenzyme deficiency: zinc, copper, and/or vitamin B-6 deficiency or damage to the small intestine mucosa, which functions as a production site for 50-70% of DAO).
It is important to differentiate between a secondary (reversible) and primary form of histamine intolerance.
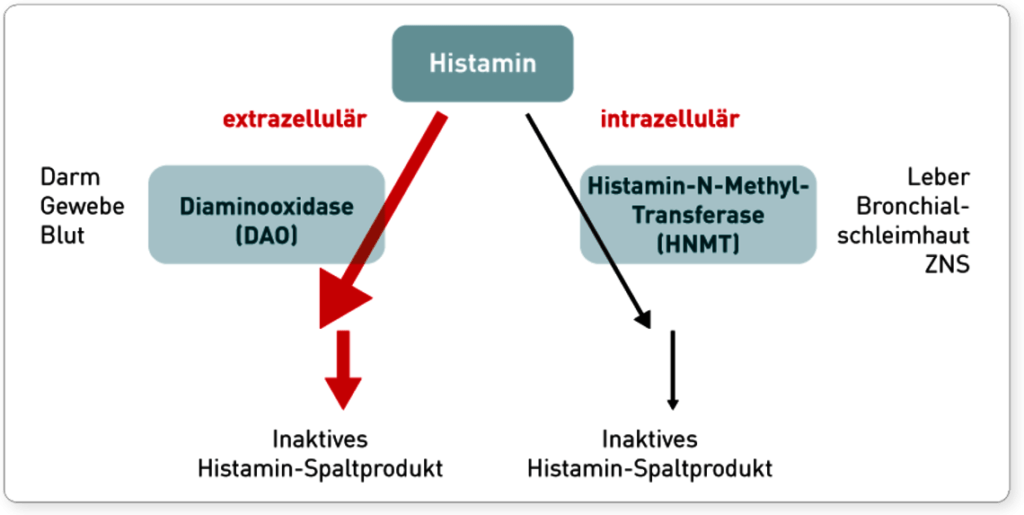
In the primary form, there are genetic changes in the histamine-degrading enzymes (DAO and HNMT). Diamine oxidase (=DAO) is responsible for the degradation of histamine in the intestine and extracellularly. However, DAO does not only degrade histamine, but also histamine-like substances, the biogenic amines. This group includes tyramine, putrescine, cadaverine and octopamine. These can themselves also play a role in a variety of medical conditions (e.g. autism, headaches, etc.). A look at the intestinal flora is therefore always recommended, even in the lack of intestinal symptoms, since these substances are formed by certain intestinal germs (see below) and, for example, in the case of a simultaneously present Leaky Gut Syndrome, they enter the blood system and develop their effect in the body.
The histamine N-methyltransferase (=HNMT) has the task of breaking down histamine in the body, e.g. in the brain. For both genes there are known polymorphisms, which can lead to a degradation disorder.
Most of the time, degradation disorders are secondary or, despite the presence of polymorphisms, it is usually possible to optimize histamine degradation through various therapeutic measures.The following graphic shows the degradation of histamine (courtesy of IMD Berlin).
Histamine intolerance or degradation disorder: Treatment
In the case of histamine intolerance, a low-histamine diet is advisable. It is practically impossible to achieve a histamine-free diet.
In addition, the coenzymes of the diamine oxidase must be checked and substituted if necessary. These are mainly copper, zinc and vitamin B-6. Under subsitution, diamine oxidase activity can sometimes improve significantly.
In addition to coenzymes, we always look at the small intestine. 50-70% of DAO is produced in the superficial cell layer (epithelium) of the small intestine. If the small intestine has a problem (e.g. a bacterial overgrowth in the small intestine (SIBO) or a leaky gut syndrome), production may be disturbed. In that case, the primary starting point for therapy is the optimization of the small intestinal environment as well as an investigation regarding the cause of the small intestinal problem.
Likewise, the intestine or the intestinal flora can be the cause of increased histamine production and biogenic amines with histamine-like effects. Here, within the framework of an imbalance in relation to the intestinal germs, increased histamine is produced by decarboxylation from the amino acid histidine, which is supplied with food, by the so-called histamine producers (Klebsiella spp., Hafnia alvei, Morganella morganii, E.coli spp. and others).
Histamine can also be determined in the stool and the dysbiosis of the intestinal bacteria can then be treated naturopathically.
Please also read our article: Diet for histamine intolerance (incl. free food list to download)
Video: Histamine intolerance / Histamine degradation disorder / MCAS
Mast cell activation syndrome (MCAD / MCAS): Symptoms
Mast cell activation syndrome is a thoroughly complex clinical picture and completely unknown to many outpatient and inpatient physicians, although it is increasingly becoming the focus of experts and university institutions. The prevalence in the population is estimated to be in the low double digits. I think the prevalence is much higher and the trend is increasing.
Many Long COVID patients as well as post VAC syndrome patients are affected by MCAS. The symptoms are so manifold due to the ubiquitous presence of histamine receptors that physicians, when hearing the many complaints of those affected, cannot imagine that there may be a mechanism behind them. Most of the patients have seen many different specialists, and each specialist treats the corresponding symptom, but they fail to see the whole picture, to the detriment and suffering of the patient. Ultimately, the doctor thinks that the symptoms must surely be partly due to the psyche of the patient.
MCAS or histamine excess in the central nervous system also leads to psychological problems and histamine activates e.g. the hypothalamic-pituitary-adrenocortical axis and in the course often leads to a chronic fatigue syndrome, sometimes with severe sleep disturbances and severe performance reductions during the day (“can’t sleep at night and am dead tired during the day”).
The symptomatology varies from patient to patient, usually only some organ systems are affected, not all, so that the presentation of the conditions is not uniform.
Mast cell activation syndrome (MCAS): Diagnosis
When MCAS is suspected, a detailed medical history is first taken, and various questionnaires may also be filled out. There are major and minor criteria for the diagnosis, but in the German health care system there is (still) no separate ICD code for the diagnosis.
The mast cell itself is the conductor of the immune system and when it disintegrates it releases over 200 messenger substances which attract further immune cells and trigger various reactions in the body. In MCAS there is an overreaction or permanent stimulation of the mast cell (by an external stimulus) and thus a permanent release of the messenger substances active in the body. This results in a mast cell permanent fire, so to speak. This can be triggered by almost anything in our environment, e.g. physical stimuli (cold/heat), microbial pathogens, environmental toxins of any kind (heavy metals, chemicals, solvents, insecticides, etc.) and much more. A causal therapy is usually not possible.
For clarification, one looks for elevated levels of relatively selective mast cell messengers. Here you can determine histamine in the blood, tryptase level (this is often normal in MCAS, usually elevated in primary mastocytosis>20ng/ml), leukotrienes in the urine and a 24 hour collection urine for N-metyhl histamine.
In conjunction with the clinic and no corroborating evidence of primary mastocytosis (criteria: lack of evidence of KITD816V-associated WHO criteria for systemic mastocytosis (SM) in bone marrow biopsy and gastrointestinal tract biopsies), one makes the diagnosis of MCAS.
Mast cell activation syndrome (MCAS): Therapy
Treatment of mast cell activation syndrome consists primarily of symptomatic administration of H1 and H2 blockers and mast cell stabilizers.
This leads, for most patients, to a significant improvement in quality of life in a timely manner. It is important to realize that primarily a stabilization of the state of health is achieved, which can be followed by a causal therapy, whereby the intestine plays a major role, as well as pathogens, toxins and the immune system.
A very great way to achieve a lot at once is the High-dose ozone therapy according to Lahodny (OHT). The OHT also has a very positive effect according to previous experiences. We clarify the known causes and try, after some stabilization, specific therapy to further stabilize the condition.
A common question: are elevated blood histamine levels indicative of histamine intolerance or MCAS?
Partially yes, but you have to do differential diagnosis. In MCAS, other mast cell mediators are often elevated (urinary leukotrienes, etc.); elevated histamine levels may be due to other causes, and the determination of histamine in the blood is only a snapshot and cannot be extrapolated to a permanent condition.
As an example, elevated histamine levels can also occur in a florid type 1 allergy, e.g., to pollen or grasses, or in parasitoses. It is also not atypical for a patient to have a combined degradation disorder due to changes in DAO or HNMT, an MCAS and a florid type 1 allergy. Any combination is (unfortunately) possible.

